Drug-resistant tuberculosis patients face dwindling treatment options
Doctors believe there is greater drug resistance and complexity of TB, which disproportionally affects immigrants.
Stephanie, 29, doesn’t know what to say when her brother, who has what his doctor says is the most drug-resistant tuberculosis ever diagnosed in the U.S., asks her what kind of life he is going to have if he can’t walk, use his hands or hear.
“I just say, ‘But you’re alive,’”
she says.
Her brother, Gary, is 37 and has
extensively drug-resistant tuberculosis (XDR TB), a rare type of
multidrug-resistant (MDR) tuberculosis that does not respond to
almost any of the drugs used to treat TB. A year ago his family
thought he would die. He still could. In November he was
admitted to the hospital for a cold, a simple sickness that for
Gary could prove deadly. He has only one lung, extreme hearing
loss and disabling nerve damage to his hands and feet that makes
it painful to walk. He suffers from paranoia and memory loss,
and his skin is covered in pimples.
The disease has
damaged his lungs; the treatment is destroying his body and
mind. Gary and Stephanie requested that their last names not be
used because of the stigma associated with the disease.
Once
the leading cause of death in the United States, tuberculosis
rates in the U.S. have been in decline for decades. Effective
drug treatments in the 1940s all but erased tuberculosis from
modern U.S. memory, until the mid-1990s, when a resurgence was
blamed on AIDS, growing drug resistance and decreased funding.
Renewed investment in TB prevention helped reverse the trend,
and numbers once again went down, with fewer than 10,000 new
cases reported in 2013. Half the cases occur in four states:
Texas, New York, Florida and California. Over the last decade
the rates of MDR TB have remained relatively constant, at about
1 percent of cases, or 86 in 2012, said Dr. Sundari Mase of the
division for tuberculosis elimination at the U.S. Centers for
Disease Control and Prevention (CDC).
But that number
is only new cases. Because of the long length of treatment,
there are twice as many at any given time if you include
patients still in treatment, said Dr. Jennifer Flood, president
of the National Tuberculosis Controllers Association and chief
of the TB control branch at the California Department of Public
Health. Even doubled, the number is small, but the threat and
effort to make sure it doesn’t spread have more to do with
the consequences than the quantity. And with MDR TB, the
repercussions are both human and economic. Treatment for MDR TB
takes years, not months. It is incredibly costly: about $260,000
(in 2010 dollars) in direct costs plus lost productivity for an
average MDR TB patient and $554,000 for an XDR TB patient,
according to a 2014 CDC study that looked at cases from 2005 to
2007. Even with treatment, 9 percent of those surveyed in the
study died.
Although there is not enough information
to make an official comparison, “anecdotally many experts
in the field feel that we are seeing greater complexity and
greater drug resistance,” said Mase. Dr. Caitlin Reed,
medical director of the inpatient TB unit at UCLA’s Olive
View Medical Center, where Gary was eventually treated, said his
case is the “most drug resistant that’s ever been
diagnosed or treated in the United States.”
Gary’s
form of XDR TB was almost untreatable. Her colleagues suggested
hospice. Instead she put him on as many as 10 to 12 often fairly
toxic antibiotics at a time. She sent him to a specialist in
Colorado to have a badly damaged lung removed. She urged the
Japanese-based Otsuka Pharmaceutical Co. to allow him to take a
new drug the company has registered in Europe and Japan but not
yet in the United States. It denied her request. Gary is no
longer contagious, but his health remains precarious. He could
still die of XDR TB.
Reed said a fellow doctor and
friend once described TB as “Ebola with wings, because you
have a disease that is extremely difficult or potentially
untreatable but you can spread it through the air.”
In
California, with MDR TB rates hovering at 1 to 2 percent of
cases annually and 27 new cases in 2013, doctors are
particularly concerned. Santa Barbara County Health Officer Dr.
Charity Thoman considers being prepared for drug-resistant TB
cases her No. 1 priority, saying it’s “more
important than planning for Ebola or anything else I
do.”
But doctors as well versed in TB as
Thoman, Reed and Flood are not the norm. As TB rates in the U.S.
continue to decline, fewer doctors are familiar with the
disease. As a result, patients are often initially misdiagnosed,
said Reed, placing both the patient and the people with whom the
patient interacts at risk.
Before being treated by
Reed, Gary received a number of confusing diagnoses. It was not
until December 2013, after years of suffering recurrent
pneumonia, that he was tested for tuberculosis, said Stephanie.
He had it. Then he didn’t have it. Then he had a
drug-resistant strain. Then he had a strain so drug-resistant,
they couldn’t treat it.
“We’re in
the 21st century. It’s not like it’s 18-something or
even the 1920s,” she said. “We’ve got machines
for freaking machines. They have robots filling orders at
Amazon. They can’t figure out a way to find out what type
of TB you have quicker?”
Often, they
can’t. Not only is diagnosis difficult because of less
medical familiarity with the disease, but also treatment and
diagnostic technology has been limited by a decline in funding
and research. A National TB Controllers Association study
revealed that 60 percent of public health TB programs in the
U.S. have eliminated staff and 25 percent have restricted
crucial activities, including those involved with TB outbreak
response. Since 2012, three major drug companies have stopped TB
research, leaving only three companies with active TB research
programs.
“Research into developing new
treatments is sort of woefully inadequate,” said Mike
Frick, TB/HIV project officer with Treatment Action Group, an
AIDS research group based in New York. “And the evidence
of that is in the past 40 years, we’ve only developed two
new drugs to treat drug-resistant tuberculosis.”
The
limited number of drugs is particularly worrying because as more
of these drugs are used around the world, more resistance to
them develops, said Flood. The concern is that new drugs will
not be developed in time to replace those for which patients
develop resistance. The lack of companies focused on developing
new drugs and producing current drugs means that normal delays
and recalls can lead to shortages, which can in turn lead to
drug resistance.
In the last two years the Centers
for Disease Control has issued seven alerts regarding shortages
of TB treatment drugs and agents used in diagnostic testing,
said Mase. According to a TB Controllers Association survey, 21
of 26 health departments treating MDR TB from 2005 to 2010
(representing about 75 percent of the U.S. TB burden) had
trouble procuring drugs for MDR TB. The majority, 90 percent,
reported resulting treatment delays and lapses, which can lead
to patients’ becoming infectious again. In 2013 there was
a shortage of a key drug used to treat TB, said Mase, causing
programs to switch regimens and start and stop treatments, all
of which can lead to the development of MDR TB.
“That
is one of the major worries with first- and second-line drug
shortages — further acquired drug resistance,” said
Mase.
For those drugs that are available, more
research is needed. In 2009, Dr. Felice Adler treated several
elementary school students in Laguna Beach, California, for
latent, or nonactive, MDR TB after their teacher developed
active MDR TB. With latent TB, a person is infected but is not
ill or contagious. About one-third of the world’s people
have latent TB; 10 percent will go on to develop the disease.
Long and toxic drug courses similar to those used to treat
active MDR TB are used to prevent latent MDR TB from becoming
active. There are no separate drugs for children, and of the 26
children in Laguna Beach who underwent treatment, only 15 were
able to complete it. Some of those who stopped did so because of
severe side effects, including hallucinations and stress to the
liver.
“We need to have more studies looking at
outcomes of treating people with these long courses of
antibiotics, specifically kids, because we just don’t have
a lot of data,” said Adler, who is director of outpatient
services for infectious diseases at Children’s Hospital of
Orange County in California. Hearing loss and nerve damage
caused by the drugs can be irreversible.
An added
concern regarding the length and toxicity of MDR TB treatment is
the risk a patient poses to others. Being isolated for months at
a time and suffering daily toxic medications for up to two years
— often after the symptoms of the disease have dissipated
— is a lot to ask of a patient. Sometimes it is too much.
In August 2014 a patient with MDR TB in Santa Barbara stopped
taking his medications and disappeared. Thoman was concerned
enough to release the patient’s name to law enforcement
and the media. The drastic measure was necessary, she said,
because she considers him “such an enormous public health
threat because he had contagious MDR TB.” The patient had
already infected multiple people, including children, and had a
rare form of MDR TB that was highly infectious. Authorities
weren’t able to locate the patient. Normally there is one
case of MDR TB in the county every other year, said Thoman. In
2014 it had three.
“MDR TB is a really, really
high priority for us,” she said. “I would say it is
probably the most high priority communicable disease that we
address in our county — that we’ve ever had in our
county. And I think that’s true for any county.”
The
100 or so new MDR TB cases cost the country $14 million
annually, said David Bryden, a TB advocacy officer with the
anti-poverty activist organization Results. On the basis of
information from a National Tuberculosis Controllers Association
survey and Denver TB expert Dr. Randall Reves’ assessment,
Bryden said that states and localities at times struggle with
tuberculosis cases and that a large school or hospital outbreak
of MDR or XDR TB would overwhelm the system.
“I
thought TB was something that happened before, like you read in
history books. It annihilated a whole bunch of people, then
there was a cure,” said Stephanie. “Apparently
it’s very much around, and you don’t know until it
hits home.”
For Stephanie, that happened last
year when Gary, the big brother who had always looked after her,
the one who wouldn’t let her leave the house in Britney
Spears–inspired crop tops as a teen, spent months in a
hospital. In the beginning, doctors entered his room in space
suits, she said. He wasn’t allowed to leave his hospital
room, and none of the drugs they were giving him were bringing
down his fever. He kept losing weight.
“Everyone
had given up on my brother, everyone,” she said.
If
he hadn’t been transferred to Reed, she believes, he would
have died. Gary is thought to have contracted XDR TB while
living in Russia. His two young children still live in Russia,
as does his girlfriend. Although Stephanie was raised in
Hollywood, her older siblings spent much of their youth in
Russia and Armenia, and Gary returned to live there for about
five years as an adult. It used to be people thought TB was
something that happened “over there” said Adler, and
“over here” we were safe.
“But
there are so many people that are foreign born in the United
States now, so there’s not really like an over there and
an over here that we can clearly differentiate anymore,”
she said.
TB rates in the U.S. disproportionately
affect certain communities, another reason declining numbers do
not tell the whole story. Foreign-born people develop TB at a
rate 13 times greater than among the U.S. born.
Chia
was born in the U.S. He had never traveled outside of the
country when he was diagnosed with MDR TB in 2013 while living
in a small town in Northern California. Chia is Asian, the
ethnic group suffering the highest TB rates in the U.S.
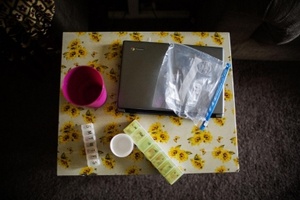
After
a month in the hospital Chia, then 20, spent almost five months
in home isolation. He had to take a leave of absence from
college and his job as a drugstore clerk. No one was allowed to
visit his house, and when he left his room, he had to wear a
mask. He passed the time playing computer games, watching movies
and Skyping with his girlfriend, who stayed faithful to him
although they were unable to see each other. It was
“really lonely, super boring,” he said.
He
said that when he finally got out, people still kept their
distance. The health department nurse who oversees his treatment
said that is common in their community. Chia asked to use only
his first name to protect his identity because of the stigma he
faces.
“I had one family that I know —
the community stopped calling them to participate in religious
ceremonies,” Chia's nurse, May Thao, said. “They
felt like they were shunned by the community they had been a
part of.”
Chia is now back at school and work
but complains of tiredness, daily nausea and numbness in his
hands and feet. Health officials administer his drugs daily and
will do so until he completes 18 months of treatment in
September 2015. They watch for long-term effects. One of the
drugs he is taking can cause nerve damage.
“The
procedures and the way they treat you and stuff like that is a
pain in the butt,” said Chia. “It’s really
harsh.”
When he first learned he had TB, he
asked, “What’s that?” He had heard of TB but
didn’t know what the big deal was. After health officials
explained the situation and told him that he had drug-resistant
TB, he understood better.
“I was like,
‘Oh, man, that’s pretty bad.’
Source:
Al Jazeera